Beyond Steady Hands: Where Surgical Robotics Beat Human Fatigue
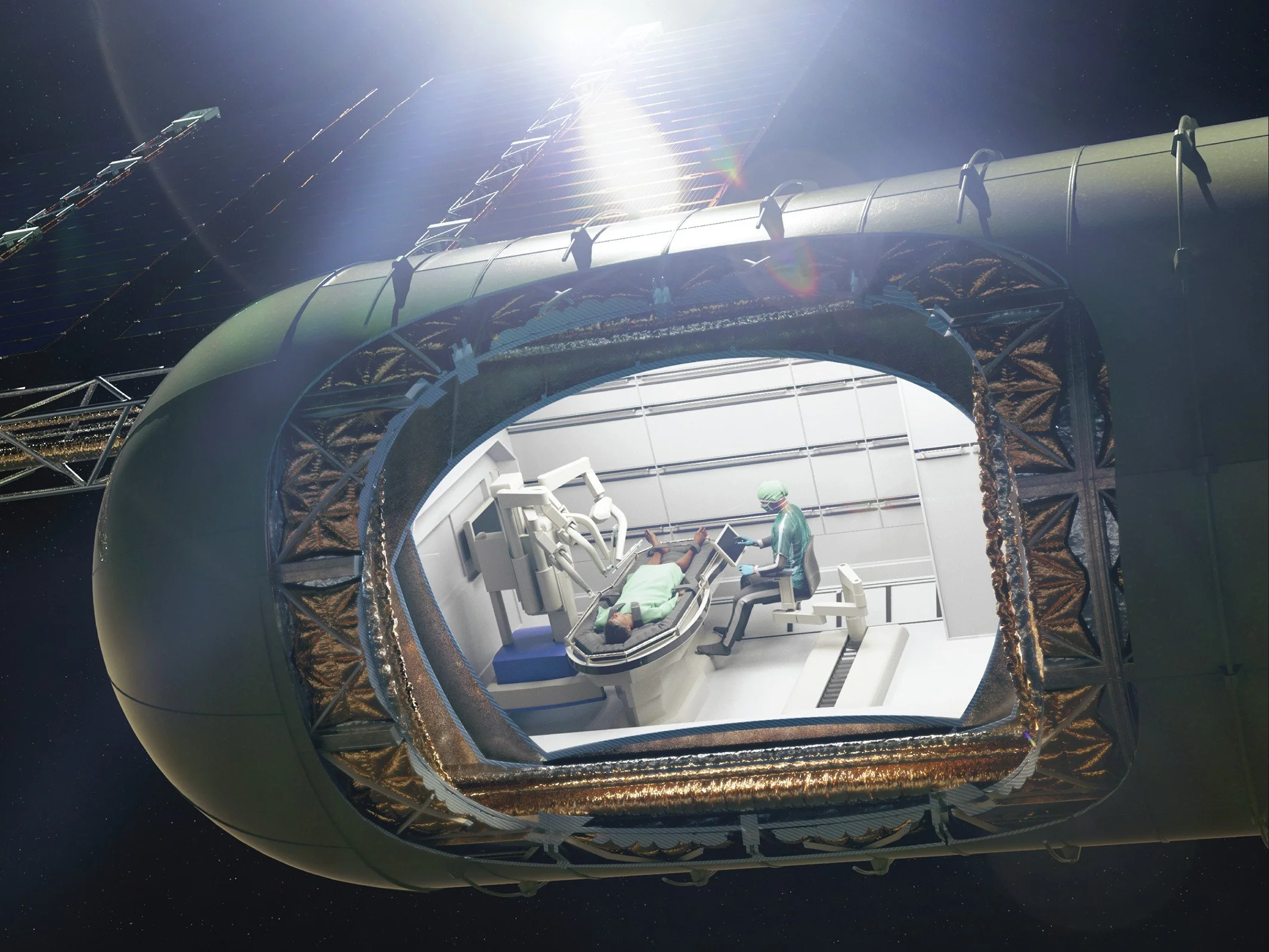
Concept art of an AI-powered surgical robot acting as a physician to perform autonomous medical procedures on astronauts in space, with minimum human intervention and staff.
Credit: NASA
Fluorescence vision, AI guidance and early autonomy are turning consistency into the real clinical edge
The strongest commercial argument for surgical robotics isn’t futuristic autonomy—it’s repeatable precision that doesn’t tire. Robots deliver steadiness on the thousandth suture as reliably as on the first, and when you pair that with better visualisation and AI-guided assistance, you start converting incremental clinical gains into dependable economics for hospitals.
Consider vision first. Intuitive’s da Vinci platforms ship with Firefly fluorescence imaging, which lets surgeons visualise blood flow and biliary structures in real time after indocyanine green dye. This is not a marketing flourish: better identification of ducts and vessels during laparoscopic procedures reduces errors at the edges of human perception, the very places where fatigue and stress can blur judgement late in a case. Firefly is now a standard part of the da Vinci value story across multiple procedures, anchoring the claim that robots can make fine anatomy more obvious when it matters most.
Layer in AI that coaches rather than replaces. Asensus Senhance’s Intelligent Surgical Unit (ISU) augments laparoscopy with surgeon-controlled eye-tracking, “Follow-Us” camera moves, smart zoom and digital tags that keep points of interest in view. The aim is to reduce cognitive load and camera wrangling while maintaining surgeon agency. Asensus is also pushing post-case analytics (e.g., AugmentOR) that surface where inefficiencies or risky manoeuvres crept in, a step toward benchmarking and training that narrows performance variance across teams and shifts. That is how “AI in the loop” earns its keep—by improving consistency across operators without demanding wholesale workflow change.
On the autonomy frontier, Johns Hopkins’ STAR project has shown that supervised autonomy can handle delicate soft-tissue tasks. In 2022, STAR performed intestinal anastomosis in animals with accuracy that matched or exceeded human baselines, adapting in real time to the squish and drift of living tissue—a historically nasty challenge for robots. More recently, Hopkins collaborators reported autonomous multi-step tasks on ex vivo organs, edging toward human trials over the next decade. The timeline is cautious, but the arc is clear: specific, bounded subtasks are moving from “human only” to “robot-first with human oversight.”
So what does the investable product look like now, not in 2035? It looks like assurance of precision under pressure. The go-to-market tone that resonates with clinical leaders is pragmatic: show how enhanced vision (e.g., Firefly) and AI guidance (e.g., ISU) together reduce error opportunities and mental load; document case-to-case variance dropping as teams adopt analytics; and commit to service levels that keep uptime high and updates safe. Early autonomy can be sold as feature-bounded gains—needle placement, camera control, suture spacing—validated in simulation and animal models, then introduced under strict governance.
Hospitals respond to evidence that travels. Bring published studies and independent validations to the pitch, but also bring operating artefacts: training pathways that blend surgeon onboarding with AI feature adoption; checklists for fluorescence-guided steps; analytics dashboards that quality teams can read without a data science degree. When the conversation stays grounded in workflow, not wonder, procurement moves faster.
Risk has to be narrated without flinching. Autonomy will fail sometimes; vision systems will mislabel or glare; AI assistants can distract if poorly configured. The counter is bounded deployment and transparent change control: turn on features in defined steps, publish before/after metrics, and give surgeons a simple “off switch” for anything that feels wrong. Robots that never tire are only an advantage if clinicians trust the assistance layers sitting on top of them.
The near-term payoff is consistency: fewer avoidable errors at the margins, steadier performance across long theatre days, and richer data to train the next cohort. That’s a commercial story hospital boards can underwrite today—precision that scales from one star surgeon to the whole service.